Health insurance is one of the most important and valuable assetsAssets refer to “all the available properties of every kind or possession of an insurance company that might be used More one can have. It provides us with the peace of mind that we are covered in case of any medical emergencies. But have you ever wondered how the claims are processed, or who is responsible for it? This is where Third Party Administrators (TPA) come in.
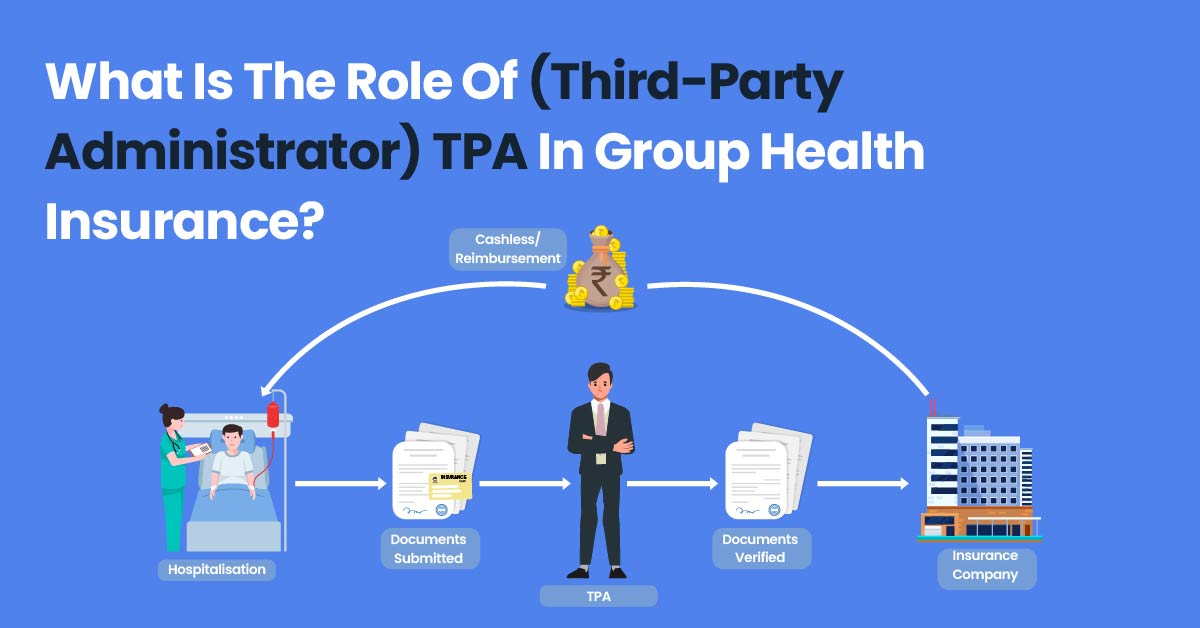
TPA plays a crucial role in the functioning of health insurance policies. They act as an intermediary between the insurance company, the policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More, and the healthcare provider. They are responsible for managing the health insurance claims process, from the beginning to the end. They help streamline the claims process and make it more efficient, helping to reduce the burden on the insurance companies and the healthcare providers.
But who are these TPAs?
Third-Party Administrators (TPAs) are independent organizations that are licensed by the Insurance Regulatory and Development Authority of India (IRDAI). They are appointed by insurance companies to provide claims management services to policyholders. They are responsible for processing health insurance claims, conducting pre-authorization, coordinating with healthcare providers, and handling all other administrative functions.
Let’s share a personal experience that highlights the critical role of TPAs in health insurance. A friend’s father was diagnosed with cancer, and his family was devastated. The entire process of getting him admitted to the hospital, undergoing various tests, and eventually starting treatment was overwhelming. But the TPA handling his health insurance policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More was a saving grace. They coordinated with the hospital, provided regular updates, and even helped them with the hospital bill settlement. Their support and guidance made a stressful time a little bit easier.
What is the role of TPA in health insurance?
The role of TPAs in health insurance is crucial. They play a vital role in ensuring that policyholders get timely access to quality healthcare and that the claims process is streamlined and efficient. They provide support and guidance to policyholders and their families during a challenging time, making the process a little bit easier.
- TPA maintains a database of policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More holders.
- TPA, issues ‘health insurance identity cards or eCards’ with unique identification numbers for each policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More.
- TPA also handles all the post policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More issues including claim settlements, cashless benefits.
- TPA studies doctor’s prescriptions to determine the pay ability of the claims, as per the policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More issued by the insurance company.
- TPA helps the insured person in filing health insurance claims, using hospital bills and documents. However, TPA is not responsible for claims rejection or acceptance.
How TPAs Work?
TPAs typically handle both cashless and reimbursement claims in health insurance policies. Here’s how TPAs work for both types of cases:
- Cashless Claims: In cashless claims, the policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More can avail medical services at a network hospital without paying any upfront charges. The TPA plays a critical role in facilitating cashless claims. Here’s how:
- The policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More informs the TPA of the planned hospitalization in a network hospital
- The TPA verifies the policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More coverage and shares the pre-authorization form with the hospital.
- The hospital fills up the pre-authorization form and shares it back with the TPA.
- The TPA reviews the pre-authorization form and approves it if it is within the policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More coverage limits.
- The hospital provides treatment to the policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More and sends the bills to the TPA for settlement.
- Reimbursement Claims: In reimbursement claims, the policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More pays for the medical services upfront and then claims a reimbursement from the insurance company. Here’s how TPAs work in reimbursement claims:
- The policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More submits the claim form, along with all the relevant documents, to the TPA.
- The TPA verifies the claim documents and checks if they are in line with the policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More coverage.
- The TPA sends the claim form and the documents to the insurance company for approval.
- Insurance company approves or denies the claim. If the claim has been denied unfairly, they the TPA will initiate an appeal process.
In both cashless and reimbursement claims, TPAs play a crucial role in ensuring that the policyholderA policyholder is an individual or entity that owns an insurance policy and pays the premium in exchange for coverage. More gets the necessary medical treatment while also ensuring that the claims are processed efficiently and accurately.
What is the importance of having a TPA in health insurance?
Here are some key reasons why having a TPA is important for policyholders:
- Efficient Claims Processing: TPAs specialize in claims processing and have the expertise to handle complex claims, which can expedite the process of getting claims paid out to policyholders.
- Reduced Administrative Burden: TPAs can handle administrative tasks like claims processing, policyAn insurance policy is a legally binding contract between an insurance company (insurer) and an individual or business (policyholder). It More issuance, and customer service, which can help reduce the administrative burden on policyholders and free up their time.
- Increased Transparency: TPAs provide regular updates and information about the status of claims, which can increase transparency and help policyholders understand the claims process better.
- Improved Customer Service: TPAs offer dedicated customer service, which can help policyholders with questions or concerns related to their policies, claims, or other administrative matters.
- Cost Savings: TPAs may negotiate lower prices with healthcare providers, which can help reduce healthcare costs for policyholders.
Overall, TPAs can help policyholders navigate the complexities of the healthcare system and make it easier for them to access the care they need.
